As maternal care in Wyoming dwindles, tribal clinics are building up resources for support
Synopsis
Obstetric services have shrunk elsewhere in Wyoming’s Fremont County. Tribal patients have greater options.
LANDER, Wyo.—When teacher Fredde Reed became pregnant with her first child in March, her choice for prenatal care was easy, she said.
“Being Native American enrolled, I can receive care at Indian Health Service,” said Reed, who is Eastern Shoshone. Reed and her wife weren’t initially certain they would stay with IHS through the birth. They wanted to explore other options in Fremont County.
But those options have dwindled significantly in recent years. Meanwhile, two clinics on the Wind River Indian Reservation — one run by IHS, a federal agency, along with Wind River Family and Community Healthcare, run by the Northern Arapaho tribe — have been building their maternal care services.
So at IHS, Reed established care with Dr. Matt Graf, a family practitioner with obstetrics training, and was assigned what felt like a whole team of staffers to keep track of her pregnancy. She also found resources through the clinic to connect with other expecting mothers.
“They are building a really good program to support moms,” Reed said. “Especially women who don’t have a lot of support.”
Reed’s experience is notable in this New Hampshire-sized county of nearly 40,000, where non-tribal residents have a single obstetric practice to visit for prenatal and delivery care. Many women travel long distances for prenatal care and to deliver because they are uncomfortable with just one option and the likelihood it creates for delivering with an on-call traveling doctor.
On the Wind River Indian Reservation, meanwhile, IHS and Wind River Family and Community Healthcare, commonly known as Wind River Cares, have made targeted efforts to ensure they meet the pregnancy and labor-related needs of their Eastern Shoshone and Northern Arapaho patients.
“I think in a lot of ways … [our patients] have more resources than the general community does,” said Dr. Laura Gibbons, who is part of a maternal health team at Wind River Cares.
Growth and needs
Gibbons is a family practice doctor with obstetrics training, meaning she can deliver babies but not perform surgeries like cesarean sections.
For more than a year, she was the only full-time OB provider at Wind River Cares, which operates clinics for tribal patients in Arapahoe, Ethete and Riverton. But late this summer, her clinic hired another family practice doctor with the same OB training, plus one who can perform C-sections.
 A woman walks into the Wind River Family and Community Healthcare clinic in Arapahoe in August 2023. (Katie Klingsporn/WyoFile)
A woman walks into the Wind River Family and Community Healthcare clinic in Arapahoe in August 2023. (Katie Klingsporn/WyoFile)
The clinic also employs two nurses dedicated solely to pregnant people, moms of young children and their kids. Lander obstetrician Dr. Thomas Dunaway, the only practicing obstetrician serving Fremont County, also contracts with the clinic for surgical needs.
It’s becoming a well-staffed team. That’s important, because as maternal care is shrinking in many parts of rural America, pregnancy-related risks are particularly high for Native people. American Indian people are more than two times as likely to die from pregnancy-related causes than non-Hispanic White people, and roughly twice as likely to experience severe maternal morbidity.
“Most of our patients are high risk,” Gibbons said, for reasons ranging from age (35 or older) to high blood pressure and gestational or preexisting diabetes.
No employees of IHS could obtain permission from the federal agency to talk to WyoFile by publication.
Unique needs
Transportation is a significant need associated with health care on the reservation — it’s a 3,500-square-mile area of scattered communities, and it’s far from urban centers where specialists are often found.
Wind River Cares operates a transportation system specifically to fill these needs, whether it’s a case of a maternal-child-health nurse picking up a patient to bring her to appointments at the clinic or the transport of a high-risk pregnant patient to see a maternal-fetal specialist in Denver.
The system is crucial, Gibbons said.
“It’d be impossible to function and provide patients the care they needed if we didn’t have that,” Gibbons said.
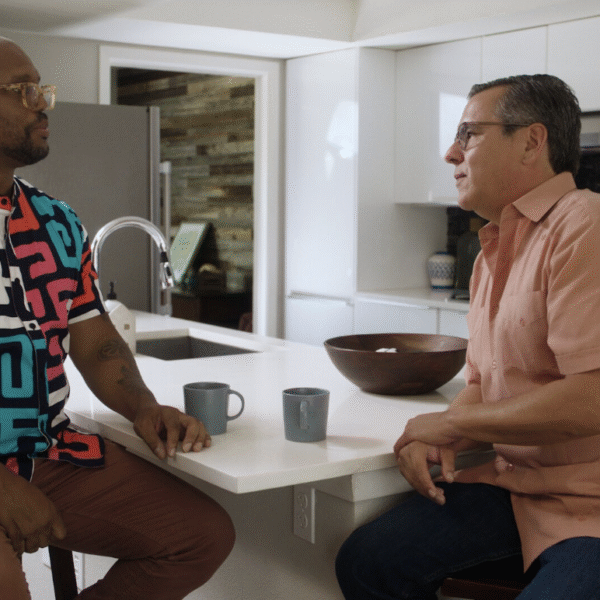
Gibbons credits Wind River Cares CEO Rick Brannan for prioritizing maternal care. Brannan, she said, was “aggressive and willing to hire more obstetrical providers for our group … I do think Wind River Cares has done a very good job of building access for our patients.”
And as a physician who spent all those months as the clinic’s sole maternal health doctor, Gibbons is relieved to see the team grow. Birth volume has bumped up in recent months, but even without that factor, she said, a bigger staff can just provide more comprehensive care.
The erosion of maternity care providers elsewhere in the county, she believes, “has just increased the pressure” to bulk up the clinic’s resources.
Still, for all the efforts, all Fremont County patients are vulnerable to the realities of rural medicine, she noted, including a provider dearth.
“It’s no secret, like, OB is not the only specialty we wish we had more of,” she said. “We’re short on doctors of all kinds.”
Happy patient
Many expecting mothers who talked to WyoFile traveled to places like Thermopolis, Casper and Salt Lake City to give birth.
Reed and her wife, in contrast, had planned to drive about a half mile from their house to Lander’s SageWest hospital, where Graf has privileges to deliver babies.
“I could give birth in Thermopolis or Jackson,” Reed said in early November. “But I really like Dr. Graf and I like the program that he’s building and I’m confident in that. So that’s kept us here.”
Plus, she said then, her December due date means “it’s going to be winter so you can’t really count on the roads being open.”
 Nurse April Bernal adjusts bedding in a labor suite in SageWest’s Lander hospital. (Katie Klingsporn/WyoFile)
Nurse April Bernal adjusts bedding in a labor suite in SageWest’s Lander hospital. (Katie Klingsporn/WyoFile)
Babies have a way of scrambling the best-laid plans, which is what happened in Reed’s case. Shortly after talking to WyoFile, she and her wife were traveling in the Denver area when her blood pressure spiked. Her doctor recommended she go in for monitoring, and Colorado medical professionals found she had severe preeclampsia — a dangerous pregnancy-related condition.
They induced Reed’s labor, five weeks short of her due date. She gave birth, and her daughter spent 13 days in the NICU, a resource Fremont County hospitals don’t have.
“We were extremely lucky to have been in the Denver area and to deliver there,” Reed said after the birth. “If we had been home, our baby would have been flown and we would have been separated.”
This article originally appeared in WyoFile, an independent nonprofit news organization focused on Wyoming people, places and policy.
When their girlfriends needed abortion care, they showed up
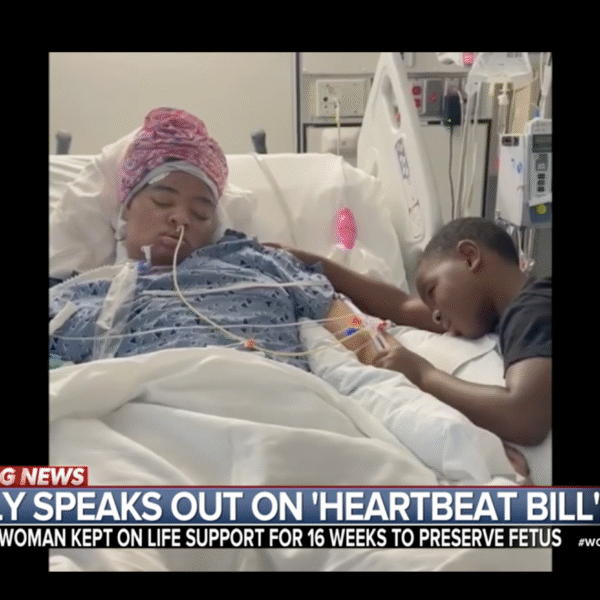
Mother whose daughter was kept on life support due to abortion ban speaks out