A Third Woman Died Under Texas’ Abortion Ban. Doctors Are Avoiding D&Cs and Reaching for Riskier Miscarriage Treatments.
Synopsis
Thirty-five-year-old Porsha Ngumezi’s case raises questions about how abortion bans are pressuring doctors to avoid standard care even in straightforward miscarriages.
Wrapping his wife in a blanket as she mourned the loss of her pregnancy at 11 weeks, Hope Ngumezi wondered why no obstetrician was coming to see her.
Over the course of six hours on June 11, 2023, Porsha Ngumezi had bled so much in the emergency department at Houston Methodist Sugar Land that she’d needed two transfusions. She was anxious to get home to her young sons, but, according to a nurse’s notes, she was still “passing large clots the size of grapefruit.”
Hope dialed his mother, a former physician, who was unequivocal. “You need a D&C,” she told them, referring to dilation and curettage, a common procedure for first-trimester miscarriages and abortions. If a doctor could remove the remaining tissue from her uterus, the bleeding would end.
But when Dr. Andrew Ryan Davis, the obstetrician on duty, finally arrived, he said it was the hospital’s “routine” to give a drug called misoprostol to help the body pass the tissue, Hope recalled. Hope trusted the doctor. Porsha took the pills, according to records, and the bleeding continued.
Three hours later, her heart stopped.
The 35-year-old’s death was preventable, according to more than a dozen doctors who reviewed a detailed summary of her case for ProPublica. Some said it raises serious questions about how abortion bans are pressuring doctors to diverge from the standard of care and reach for less-effective options that could expose their patients to more risks. Doctors and patients described similar decisions they’ve witnessed across the state.
It was clear Porsha needed an emergency D&C, the medical experts said. She was hemorrhaging and the doctors knew she had a blood-clotting disorder, which put her at greater danger of excessive and prolonged bleeding. “Misoprostol at 11 weeks is not going to work fast enough,” said Dr. Amber Truehart, an OB-GYN at the University of New Mexico Center for Reproductive Health. “The patient will continue to bleed and have a higher risk of going into hemorrhagic shock.” The medical examiner found the cause of death to be hemorrhage.
D&Cs — a staple of maternal health care — can be lifesaving. Doctors insert a straw-like tube into the uterus and gently suction out any remaining pregnancy tissue. Once the uterus is emptied, it can close, usually stopping the bleeding.
But because D&Cs are also used to end pregnancies, the procedure has become tangled up in state legislation that restricts abortions. In Texas, any doctor who violates the strict law risks up to 99 years in prison. Porsha’s is the fifth case ProPublica has reported in which women died after they did not receive a D&C or its second-trimester equivalent, a dilation and evacuation; three of those deaths were in Texas.
Texas doctors told ProPublica the law has changed the way their colleagues see the procedure; some no longer consider it a first-line treatment, fearing legal repercussions or dissuaded by the extra legwork required to document the miscarriage and get hospital approval to carry out a D&C. This has occurred, ProPublica found, even in cases like Porsha’s where there isn’t a fetal heartbeat or the circumstances should fall under an exception in the law. Some doctors are transferring those patients to other hospitals, which delays their care, or they’re defaulting to treatments that aren’t the medical standard.
Misoprostol, the medicine given to Porsha, is an effective method to complete low-risk miscarriages but is not recommended when a patient is unstable. The drug is also part of a two-pill regimen for abortions, yet administering it may draw less scrutiny than a D&C because it requires a smaller medical team and because the drug is commonly used to induce labor and treat postpartum hemorrhage. Since 2022, some Texas women who were bleeding heavily while miscarrying have gone public about only receiving medication when they asked for D&Cs. One later passed out in a pool of her own blood.
“Stigma and fear are there for D&Cs in a way that they are not for misoprostol,” said Dr. Alison Goulding, an OB-GYN in Houston. “Doctors assume that a D&C is not standard in Texas anymore, even in cases where it should be recommended. People are afraid: They see D&C as abortion and abortion as illegal.”

Doctors and nurses involved in Porsha’s care did not respond to multiple requests for comment.
Several physicians who reviewed the summary of her case pointed out that Davis’ post-mortem notes did not reflect nurses’ documented concerns about Porsha’s “heavy bleeding.” After Porsha died, Davis wrote instead that the nurses and other providers described the bleeding as “minimal,” though no nurses wrote this in the records. ProPublica tried to ask Davis about this discrepancy. He did not respond to emails, texts or calls.
Houston Methodist officials declined to answer a detailed list of questions about Porsha’s treatment. They did not comment when asked whether Davis’ approach was the hospital’s “routine.” A spokesperson said that “each patient’s care is unique to that individual.”
“All Houston Methodist hospitals follow all state laws,” the spokesperson added, “including the abortion law in place in Texas.”
“We Need to See the Doctor”

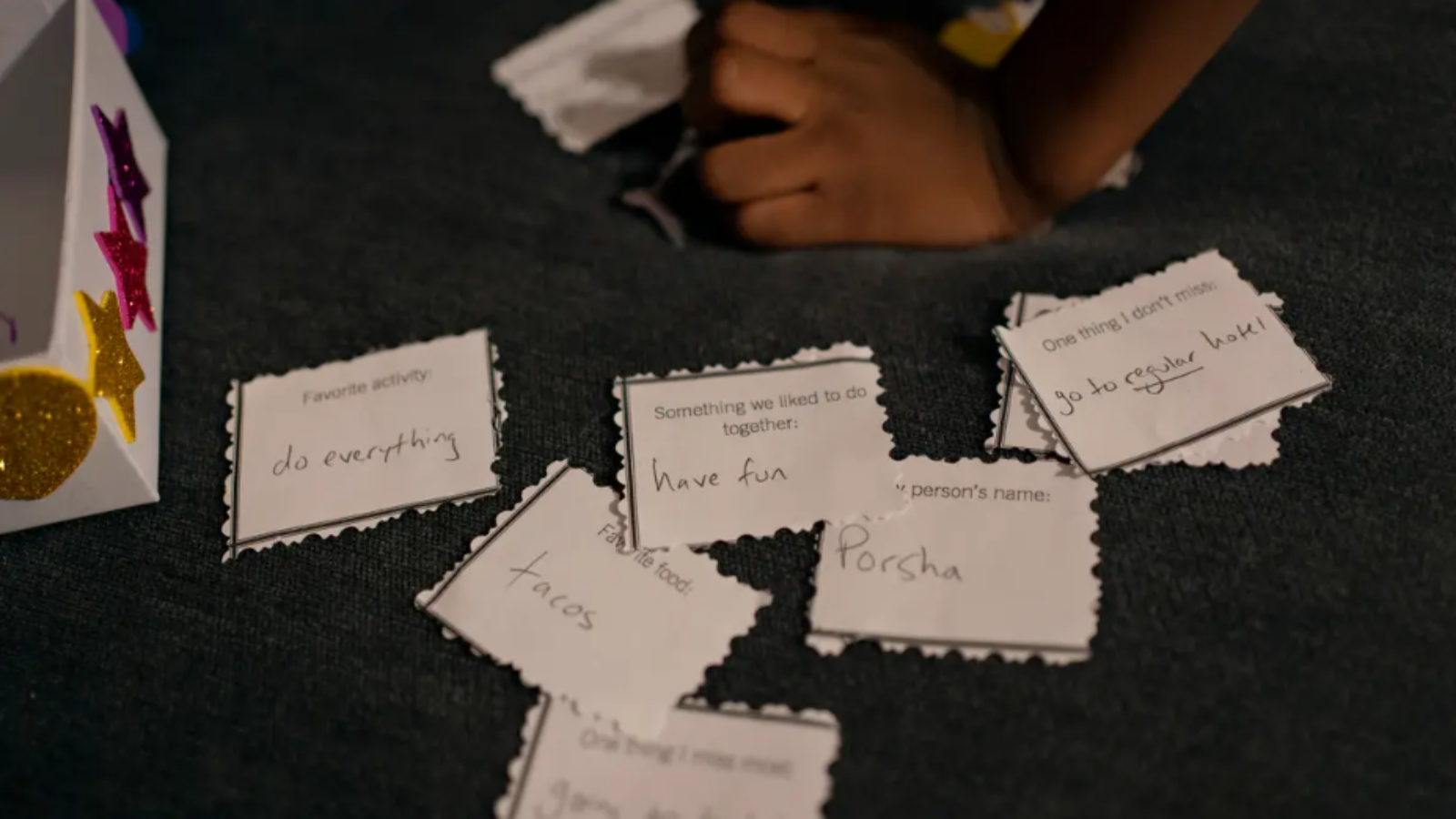
Hope marveled at the energy Porsha had for their two sons, ages 5 and 3. Whenever she wasn’t working, she was chasing them through the house or dancing with them in the living room. As a finance manager at a charter school system, she was in charge of the household budget. As an engineer for an airline, Hope took them on flights around the world — to Chile, Bali, Guam, Singapore, Argentina.
The two had met at Lamar University in Beaumont, Texas. “When Porsha and I began dating,” Hope said, “I already knew I was going to love her.” She was magnetic and driven, going on to earn an MBA, but she was also gentle with him, always protecting his feelings. Both were raised in big families and they wanted to build one of their own.
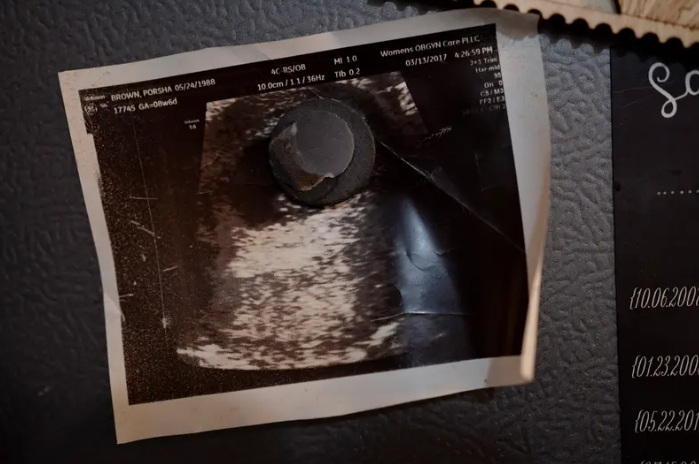
When he learned Porsha was pregnant again in the spring of 2023, Hope wished for a girl. Porsha found a new OB-GYN who said she could see her after 11 weeks. Ten weeks in, though, Porsha noticed she was spotting. Over the phone, the obstetrician told her to go to the emergency room if it got worse.
To celebrate the end of the school year, Porsha and Hope took their boys to a water park in Austin, and as they headed back, on June 11, Porsha told Hope that the bleeding was heavier. They decided Hope would stay with the boys at home until a relative could take over; Porsha would drive to the emergency room at Houston Methodist Sugar Land, one of seven community hospitals that are part of the Houston Methodist system.
At 6:30 p.m, three hours after Porsha arrived at the hospital, she saw huge clots in the toilet. “Significant bleeding,” the emergency physician wrote. “I’m starting to feel a lot of pain,” Porsha texted Hope. Around 7:30 p.m., she wrote: “She said I might need surgery if I don’t stop bleeding,” referring to the nurse. At 7:50 p.m., after a nurse changed her second diaper in an hour: “Come now.”
Still, the doctor didn’t mention a D&C at this point, records show. Medical experts told ProPublica that this wait-and-see approach has become more common under abortion bans. Unless there is “overt information indicating that the patient is at significant risk,” hospital administrators have told physicians to simply monitor them, said Dr. Robert Carpenter, a maternal-fetal medicine specialist who works in several hospital systems in Houston. Methodist declined to share its miscarriage protocols with ProPublica or explain how it is guiding doctors under the abortion ban.
As Porsha waited for Hope, a radiologist completed an ultrasound and noted that she had “a pregnancy of unknown location.” The scan detected a “sac-like structure” but no fetus or cardiac activity. This report, combined with her symptoms, indicated she was miscarrying.
But the ultrasound record alone was less definitive from a legal perspective, several doctors explained to ProPublica. Since Porsha had not had a prenatal visit, there was no documentation to prove she was 11 weeks along. On paper, this “pregnancy of unknown location” diagnosis could also suggest that she was only a few weeks into a normally developing pregnancy, when cardiac activity wouldn’t be detected. Texas outlaws abortion from the moment of fertilization; a record showing there is no cardiac activity isn’t enough to give physicians cover to intervene, experts said.
Dr. Gabrielle Taper, who recently worked as an OB-GYN resident in Austin, said that she regularly witnessed delays after ultrasound reports like these. “If it’s a pregnancy of unknown location, if we do something to manage it, is that considered an abortion or not?” she said, adding that this was one of the key problems she encountered. After the abortion ban went into effect, she said, “there was much more hesitation about: When can we intervene, do we have enough evidence to say this is a miscarriage, how long are we going to wait, what will we use to feel definitive?”
At Methodist, the emergency room doctor reached Davis, the on-call OB-GYN, to discuss the ultrasound, according to records. They agreed on a plan of “observation in the hospital to monitor bleeding.”
Around 8:30 p.m., just after Hope arrived, Porsha passed out. Terrified, he took her head in his hands and tried to bring her back to consciousness. “Babe, look at me,” he told her. “Focus.” Her blood pressure was dipping dangerously low. She had held off on accepting a blood transfusion until he got there. Now, as she came to, she agreed to receive one and then another.
By this point, it was clear that she needed a D&C, more than a dozen OB-GYNs who reviewed her case told ProPublica. She was hemorrhaging, and the standard of care is to vacuum out the residual tissue so the uterus can clamp down, physicians told ProPublica.
“Complete the miscarriage and the bleeding will stop,” said Dr. Lauren Thaxton, an OB-GYN who recently left Texas.
“At every point, it’s kind of shocking,” said Dr. Daniel Grossman, a professor of obstetrics and gynecology at the University of California, San Francisco who reviewed Porsha’s case. “She is having significant blood loss and the physician didn’t move toward aspiration.”
All Porsha talked about was her devastation of losing the pregnancy. She was cold, crying and in extreme pain. She wanted to be at home with her boys. Unsure what to say, Hope leaned his chest over the cot, passing his body heat to her.
At 9:45 p.m., Esmeralda Acosta, a nurse, wrote that Porsha was “continuing to pass large clots the size of grapefruit.” Fifteen minutes later, when the nurse learned Davis planned to send Porsha to a floor with fewer nurses, she “voiced concern” that he wanted to take her out of the emergency room, given her condition, according to medical records.
At 10:20 p.m., seven hours after Porsha arrived, Davis came to see her. Hope remembered what his mother had told him on the phone earlier that night: “She needs a D&C.” The doctor seemed confident about a different approach: misoprostol. If that didn’t work, Hope remembers him saying, they would move on to the procedure.
A pill sounded good to Porsha because the idea of surgery scared her. Davis did not explain that a D&C involved no incisions, just suction, according to Hope, or tell them that it would stop the bleeding faster. The Ngumezis followed his recommendation without question. “I’m thinking, ‘He’s the OB, he’s probably seen this a thousand times, he probably knows what’s right,’” Hope said.
But more than a dozen doctors who reviewed Porsha’s case were concerned by this recommendation. Many said it was dangerous to give misoprostol to a woman who’s bleeding heavily, especially one with a blood clotting disorder. “That’s not what you do,” said Dr. Elliott Main, the former medical director for the California Maternal Quality Care Collaborative and an expert in hemorrhage, after reviewing the case. “She needed to go to the operating room.” Main and others said doctors are obliged to counsel patients on the risks and benefits of all their options, including a D&C.
Performing a D&C, though, attracts more attention from colleagues, creating a higher barrier in a state where abortion is illegal, explained Goulding, the OB-GYN in Houston. Staff are familiar with misoprostol because it’s used for labor, and it only requires a doctor and a nurse to administer it. To do a procedure, on the other hand, a doctor would need to find an operating room, an anesthesiologist and a nursing team. “You have to convince everyone that it is legal and won’t put them at risk,” said Goulding. “Many people may be afraid and misinformed and refuse to participate — even if it’s for a miscarriage.”
Davis moved Porsha to a less-intensive unit, according to records. Hope wondered why they were leaving the emergency room if the nurse seemed so worried. But instead of pushing back, he rubbed Porsha’s arms, trying to comfort her. The hospital was reputable. “Since we were at Methodist, I felt I could trust the doctors.”
On their way to the other ward, Porsha complained of chest pain. She kept remarking on it when they got to the new room. From this point forward, there are no nurse’s notes recording how much she continued to bleed. “My wife says she doesn’t feel right, and last time she said that, she passed out,” Hope told a nurse. Furious, he tried to hold it together so as not to alarm Porsha. “We need to see the doctor,” he insisted.
Her vital signs looked fine. But many physicians told ProPublica that when healthy pregnant patients are hemorrhaging, their bodies can compensate for a long time, until they crash. Any sign of distress, such as chest pain, could be a red flag; the symptom warranted investigation with tests, like an electrocardiogram or X-ray, experts said. To them, Porsha’s case underscored how important it is that doctors be able to intervene before there are signs of a life-threatening emergency.
But Davis didn’t order any tests, according to records.
Around 1:30 a.m., Hope was sitting by Porsha’s bed, his hands on her chest, telling her, “We are going to figure this out.” They were talking about what she might like for breakfast when she began gasping for air.
“Help, I need help!” he shouted to the nurses through the intercom. “She can’t breathe.”
“All She Needed”
Hours later, Hope returned home in a daze. “Is mommy still at the hospital?” one of his sons asked. Hope nodded; he couldn’t find the words to tell the boys they’d lost their mother. He dressed them and drove them to school, like the previous day had been a bad dream. He reached for his phone to call Porsha, as he did every morning that he dropped the kids off. But then he remembered that he couldn’t.
Friends kept reaching out. Most of his family’s network worked in medicine, and after they said how sorry they were, one after another repeated the same message. All she needed was a D&C, said one. They shouldn’t have given her that medication, said another. It’s a simple procedure, the callers continued. We do this all the time in Nigeria.
Since Porsha died, several families in Texas have spoken publicly about similar circumstances. This May, when Ryan Hamilton’s wife was bleeding while miscarrying at 13 weeks, the first doctor they saw at Surepoint Emergency Center Stephenville noted no fetal cardiac activity and ordered misoprostol, according to medical records. When they returned because the bleeding got worse, an emergency doctor on call, Kyle Demler, said he couldn’t do anything considering “the current stance” in Texas, according to Hamilton, who recorded his recollection of the conversation shortly after speaking with Demler. (Neither Surepoint Emergency Center Stephenville nor Demler responded to several requests for comment.)
They drove an hour to another hospital asking for a D&C to stop the bleeding, but there, too, the physician would only prescribe misoprostol, medical records indicate. Back home, Hamilton’s wife continued bleeding until he found her passed out on the bathroom floor. “You don’t think it can really happen like that,” said Hamilton. “It feels like you’re living in some sort of movie, it’s so unbelievable.”
Across Texas, physicians say they blame the law for interfering with medical care. After ProPublica reported last month on two women who diedafter delays in miscarriage care, 111 OB-GYNs sent a letter to Texas policymakers, saying that “the law does not allow Texas women to get the lifesaving care they need.”
Dr. Austin Dennard, an OB-GYN in Dallas, told ProPublica that if one person on a medical team doubts the doctor’s choice to proceed with a D&C, the physician might back down. “You constantly feel like you have someone looking over your shoulder in a punitive, vigilante type of way.”
The criminal penalties are so chilling that even women with diagnoses included in the law’s exceptions are facing delays and denials. Last year, for example, legislators added an update to the ban for patients diagnosed with previable premature rupture of membranes, in which a patient’s water breaks before a fetus can survive. Doctors can still face prosecution for providing abortions in those cases, but they are offered the chance to justify themselves with what’s called an “affirmative defense,” not unlike a murder suspect arguing self defense. This modest change has not stopped some doctors from transferring those patients instead of treating them; Dr. Allison Gilbert, an OB-GYN in Dallas, said doctors send them to her from other hospitals. “They didn’t feel like other staff members would be comfortable proceeding with the abortion,” she said. “It’s frustrating that places still feel like they can’t act on some of these cases that are clearly emergencies.” Women denied treatment for ectopic pregnancies, another exception in the law, have filed federal complaints.
In response to ProPublica’s questions about Houston Methodist’s guidance on miscarriage management, a spokesperson, Gale Smith, said that the hospital has an ethics committee, which can usually respond within hours to help physicians and patients make “appropriate decisions” in compliance with state laws.
After Porsha died, Davis described in the medical record a patient who looked stable: He was tracking her vital signs, her bleeding was “mild” and she was “said not to be in distress.” He ordered bloodwork “to ensure patient wasn’t having concerning bleeding.” Medical experts who reviewed Porsha’s case couldn’t understand why Davis noted that a nurse and other providers reported “decreasing bleeding” in the emergency department when the record indicated otherwise. “He doesn’t document the heavy bleeding that the nurse clearly documented, including the significant bleeding that prompted the blood transfusion, which is surprising,” Grossman, the UCSF professor, said.
Patients who are miscarrying still don’t know what to expect from Houston Methodist.
This past May, Marlena Stell, a patient with symptoms nearly identical to Porsha’s, arrived at another hospital in the system, Houston Methodist The Woodlands. According to medical records, she, too, was 11 weeks along and bleeding heavily. An ultrasound confirmed there was no fetal heartbeat and indicated the miscarriage wasn’t complete. “I assumed they would do whatever to get the bleeding to stop,” Stell said.
Instead, she bled for hours at the hospital. She wanted a D&C to clear out the rest of the tissue, but the doctor gave her methergine, a medication that’s typically used after childbirth to stop bleeding but that isn’t standard care in the middle of a miscarriage, doctors told ProPublica. “She had heavy bleeding, and she had an ultrasound that’s consistent with retained products of conception.” said Dr. Jodi Abbott, an associate professor of obstetrics and gynecology at Boston University School of Medicine, who reviewed the records. “The standard of care would be a D&C.”
Stell says that instead, she was sent home and told to “let the miscarriage take its course.” She completed her miscarriage later that night, but doctors who reviewed her case, so similar to Porsha’s, said it showed how much of a gamble physicians take when they don’t follow the standard of care. “She got lucky — she could have died,” Abbott said. (Houston Methodist did not respond to a request for comment on Stell’s care.)
It hadn’t occurred to Hope that the laws governing abortion could have any effect on his wife’s miscarriage. Now it’s the only explanation that makes sense to him. “We all know pregnancies can come out beautifully or horribly,” Hope told ProPublica. “Instead of putting laws in place to make pregnancies safer, we created laws that put them back in danger.”
For months, Hope’s youngest son didn’t understand that his mom was gone. Porsha’s long hair had been braided, and anytime the toddler saw a woman with braids from afar, he would take off after her, shouting, “That’s mommy!”
A couple weeks ago, Hope flew to Amsterdam to quiet his mind. It was his first trip without Porsha, but as he walked the city, he didn’t know how to experience it without her. He kept thinking about how she would love the Christmas lights and want to try all the pastries. How she would have teased him when he fell asleep on a boat tour of the canals. “I thought getting away would help,” he wrote in his journal. “But all I’ve done is imagine her beside me.”
Mariam Elba and Lexi Churchill contributed research.
ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.

A reverend was in danger of bleeding out. Missouri’s abortion ban made her afraid to get the help she needed.

A North Texas nurse wanted to ease her baby’s suffering. She had to leave Texas to do it.